In the operating theatre the anaesthetic machine, typically attached to a circle system in adults, fulfills most of the requirements of an ideal device for both preoxygenation (PreOx) & subsequent positive pressure ventilation for reoxygenation (ReOx) during the process of airway management. It provides high concentration oxygen through a low resistance circuit that retains a ‘feel’ for the presence of leaks or changes in airway/circuit/lung compliance by virtue of its soft collapsible bag.
Outside of the operating theatre in sites such as the emergency department (ED), intensive care unit (ICU), on the wards – or even as close as the post-anaesthetic care unit (PACU), where anaesthetic machines are not always immediately available, a variety of different devices are used for PreOx & ReOx of patients requiring airway management.
The most common devices used for this purpose are:
- Non-rebreathing mask (NRM) combined with oxygen supplementation via nasal prongs from a separate oxygen source. This is increasingly being used in ED’s.
- Self inflating bag-valve-mask device (BVM). This is the most common device in use and is found in many ED’s, ICU’s & PACU.
- Mapleson B Circuit. Once a common device in the PACU it is increasingly being replaced by BVMs.
The BVM & Mapleson B utilise masks which are variations on that depicted below and require tight application and a seal around their perimeter for proper function. They can be used to provide PreOx as well as for positive pressure ventilation during ReOx.

The NRM utilises a mask which does not require a tight seal for PreOx (provided it is combined with supplementary high flow nasal or buccal oxygen) but cannot be used for ReOx in the apnoeic patient.

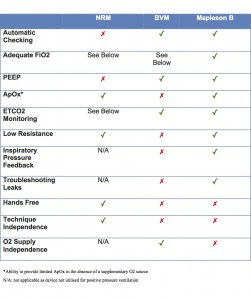
Due to the variations in mask type, as well as for other reasons, these devices differ in their ability to meet the “ideal” performance characteristics provided by an anaesthetic circle system. This post examines the merits and disadvantages of the use of each of these devices for in hospital oxygen delivery in the period surrounding advanced airway management. For each device, the following criteria will be examined:
1. Automatic Checking: when the same device is used for PreOx as for subsequent ReOx by mask ventilation post-induction (when appropriate) it enforces an “automatic check” of some aspects relating to the ventilation device used. This is not intended to usurp the utility of formalised checklists or preparation procedures for airway management but provides some level of redundancy by integrating some checks into routine practice, making them more difficult to overlook even under time pressured circumstances where formal checklists are sometimes omitted. Use of the same device for PreOx & ReOx allows this level of automatic checking of the following:
Availability: at the most basic level use of the same device for both PreOx & ReOx means that availability of the ventilation device is confirmed during the PreOx process. PreOx cannot be undertaken without the intended ventilation device being present making its availbility is difficult to overlook.
Face Mask Seal: use of the same device for both PreOx & ventilation allows the integrity of the face mask seal to be assessed during the preoxygenation process via visual assessement of mask fit, morphology of the capnography waveform (provided this is attached during preoxygenation) and observation of filling of reservoir bag (where a collapsible bag is used). Whilst good mask seal during preoxygenation does not always guarantee good mask seal post induction (although this will usually be the case), inability to obtain a seal in a cooperative patient pre-induction will usually translate to persistent inability to obtain a seal post-induction (as well as drastically reducing the FiO2 delivered during PreOx, making it much less effective). Thus assessment of the face mask seal during the PreOx process provides an opportunity to implement strategies to eliminate leaks (eg. change of face mask type/size or technique) prior to becoming dependent on a good seal to positively pressure ventilate the patient post induction – when the inability to ventilate the patient potentially places them at risk of critical desaturation if other non-surgical airway (NSA) techniques are also unsuccessful. Additionally where the cause of a leak around the face mask involves suboptimal technique, identification of this allows the airway operator to nuance and optimise their technique for application of the mask. In other words it provides an opportunity to practice the technique of getting a seal with a face mask on every patient induced, even though face mask ventilation may never need to be implemented in most of these. Enabling clinicians to maintain & develop face mask skills has benefits which can extend well beyond those afforded just to the individual patients on whom they are practised. This is particularly important for clinicians who primarily practice airway management on unfasted, emergency patients via rapid sequence induction (RSI) which does not classically involve face mask ventilation. Anaesthetists managing fasted, elective patients may accumulate a total of upto 10-20mins of practice at face mask ventilation over the course of a day, prior to inserting a laryngeal mask or whilst waiting for non-depolarising muscle relaxants to take effect before intubating. Conversely, the opportunities for emergency & intensive care clinicians performing RSI to practice face mask ventilation on patients are largely restricted to circumstances where intubation has been unsuccessful. These circumstances are both infrequent & stressful, factors which may limit the ability of such clinicians to develop proficiency in these skills. Clinicians solely performing emergency airway management are thus much more dependent on the opportunities provided by PreOx to gain feedback in their ability to obtain an adequate face mask seal and to finesse the subtleties of their technique in order to maintain & develop this important and difficult skill.
It is worth noting that use of the same device for both PreOx & ReOx does not confirm the function of the device for positive pressure ventilation and thus does not negate the need to check equipment for appropriate assembly, valve function, absence of leaks, etc.
2. Adequate Inspired Oxygen Concentration (FiO2): optimal PreOx requires delivery of an FiO2 exceeding 90%. This is dependent on the ability of the device to provide this and the absence of leaks which might dilute this via entrainment of room air. Ideally the ability of the device to deliver high FiO2 should be maintained in the face of patient hyperventilation. The ability of various devices to provide a high FiO2 under a variety of conditions is examined in more detail here.
3. PEEP: application of PEEP during preoxygenation improves the safe apnoea time post induction. Thus ability of O2 delivery devices to provide PEEP is a desirable feature if they are to be used for PreOx. Further information regarding use of PEEP during PreOx is available here.
4. Apnoeic Oxygenation: the use of apnoeic oxygenation (ApOx) techniques can significantly prolong the safe apnoea time provided a patent airway exists and there is an ongoing source of 100% oxygen. Achieving ApOx during attempts at laryngoscopy (when the O2 delivery device used for preoxygenation has been removed) requires an O2 source such as nasal or buccal cannulae which can remain applied during airway instrumentation. Even when these supplementary oxygen sources have not been utilised, however, some of the benefits of ApOx can still be yielded during the apnoeic period of a RSI when the oxygen delivery device remains applied, post induction & prior to instrumentation of the airway. This is only possible though, if the O2 delivery device provides an ongoing oxygen supply in the absence of ventilation. Given that optimal implementation of techniques for ApOx requires supplementary oxygen sources, which overcome this issue anyway, when these are being utilised the practical benefit of this characteristic of oxygen delivery devices is minimal. Further details on the rationale and techniques for apnoeic oxygenation are available here.
5. End-Tidal Carbon Dioxide (ETCO2) Monitoring: the importance of ETCO2 monitoring in confirming correct placement of advanced airway devices is well recognised. There are additional benefits to being able to monitor ETCO2 via the device that is to be used for PreOx +/- subsequent face mask ventilation.
Availability & Function: application of ETCO2 monitoring during preoxygenation confirms the availability and operation of the capnography device so that its absence does not interfere with subsequent confirmation of ability to positive pressure ventilate the alveoli post-induction.
Face Mask Seal: as mentioned above, CO2 waveform morphology can be used to help indicate adequacy of seal with a face mask, thereby improving the ability to eliminate leaks prior to induction and providing important routine feedback to help maintain/develop facemask application technique.
Airway Patency: although the primary role of ETCO2 monitoring is typically seen to be confirmation of tracheal placement of an endotracheal tube, it provides this confirmation by identifying the return of alveolar gas during expiration and thus provides an indication of airway patency and the ability to ventilate the alveoli using any oxygen delivery device to which it is attached. As such having ETCO2 monitoring already attached & operational remains useful even if intubation is unsuccessful as it provides immediate confirmation of the ability to positive pressure ventilate the alveoli using a face mask when this is adopted as a rescue technique, without the need to add the CO2 monitor into the circuit during a period of stress, when this may be overlooked, difficult or unnecessarily time consuming. This provides a further rationale for having ETCO2 monitoring connected from the outset and not only attached after an endotracheal tube has been placed.
6. Low Resistance: oxygen delivery devices which have lightweight or absent valves produce less resistance to breathing in the spontaneously ventilating patient during PreOx.
7. Feedback on Inspiratory Pressures: during positive pressure ventilation (ReOx) with O2 delivery devices that have a soft collapsible bag (rather than a self-inflating bag) with which to ventilate, the compliance of the bag provides sensitive feedback on the pressures being generated during inspiration which can be valuable in order to gauge the presence of the following:
Overly vigorous face mask ventilation: producing unnecessarily high airway pressures which may predispose to gastric insufflation and regurgitation/aspiration.
Partial airway obstruction: resulting in increased inspiratory pressures in order to overcome the obstruction. Inspiratory pressures may be able to be reduced and alveolar ventilation improved, if the partial obstruction is identified and relieved by implementation of further optimsation manoeuvres.
Decreased lung compliance: due to lung pathology such as pulmonary oedema or bronchospasm resulting in increased ventilation pressures.
8. Troubleshooting Leaks: during facemask ventilation, the reason for the occurrence of leaks may be divided into 2 broad categories:
1. Primary Leaks: these occur due to an inadequate seal pressure allowing gas to escape around the perimeter of the mask. Primary leaks may also occur due to equipment faults allowing gas to leak through holes/disconnections in the face mask or oxygen delivery device itself. Primary leaks require interventions to seal the route by which escape of gas is occurring.
2. Secondary Leaks: these occur due to airway obstruction which is unable to be overcome, resulting in higher than normal inspiratory pressures which exceed what would otherwise have been an adequate seal pressure. Thus even with ideal application of a face mask, attempts at positive ventilation of a completely obstructed airway must ultimately lead to a escape of gas around the perimeter of the mask – as gas is being forced into a blind ending passage and “something’s gotta give”. Secondary leaks require interventions to improve airway patency.
Leaving equipment faults to one side (as the site of gas escape usually immediately identifies them as primary leaks), in the presence of both primary & secondary leaks, gas escapes around the perimeter of the mask and impaired or absent alveolar ventilation results. The ability to distinguish between these two scenarios, however, is of critical importance as it informs the airway operator as to the most appropriate strategy to efficiently overcome the problem. In a primary leak, interventions to improve airway patency are unlikely to be of assistance and the appropriate strategy is to adjust facemask technique so as to improve the seal – otherwise the patient will not be able to be ventilated. In contrast when faced with a secondary leak interventions to improve the seal around the facemask are less likely to be of assistance in restoring ability to positive pressure ventilate unless interventions to overcome the airway obstruction are also implemented. O2 delivery devices which have a soft collapsible bag to facilitate ventilation enable these two situations to be clearly distinguished. Using such devices primary leaks are identifiable during ReOx (and often during PreOx as well, as mentioned above with respect to automatic checking of face mask seal), by collapse of the reservoir bag, indicating that attention needs to be directed to adjusting face mask technique so as to provide an improved seal around the perimeter of the mask. In the presence of a “secondary leak” however, the soft bag will remain pressurised and inflated, indicating that the seal around the face mask is likely to be adequate and attention neeeds to be directed towards techniques to improve airway patency during facemask ventilation. In contrast, devices with a self-inflating bag do not allow this distinction to be made as, by definition, the self-inflating bag will remain inflated independent of the ability to pressurise the airway. In addition the stiffer material of the self-inflating bag provides limited feedback about the pressure being generated during inspiration and severely limits the ability to identify airway obstruction as the cause of a facemask leak and distinguish between primary and secondary leaks.
9. Hands Free:
Devices such as NRM’s allow PreOx to be conducted “hands free” whilst other preparations for airway management are being made. This may be beneficial in an environment where staff are so limited that it is not possible to allocate the tasks of preoxygenation & preparation to separate individuals. It is important to recognise, however, that the time saved is at most 3 minutes (for full preoxygenation) and that in allowing the airway operator to take on other tasks, “hands free” preoxygenation makes the airway operator vulnerable to potential distractions which divert their attention from the vigilant observation of a patient whose already compromised airway/breathing/conscious state may have been the trigger for them requiring intubation in the first instance. It could be argued that in many clinical situations, once the decision to non-electively intubate a patient has been made, the best practice would be for the airway operator to simply monitor the patient’s ABC’s whilst undertaking PreOx and allow other staff members to prepare resources.
10. Technique Independence:
Devices such as NRMs that, when used in combination with high flow nasal oxygen, are capable of maintaining a sufficiently high FiO2 without relying on tight seal around the edge of the mask, can achieve effective PreOx without being dependent on nuanced techniques for mask application. This clearly presents an advantage for the “claustrophobic” patient who might not tolerate the firm application of pressure required to get a complete seal with the types of face mask used with BVM’s or Mapleson’s. Similarly the combative/uncooperative patient who might otherwise pull a facemask requiring a tight seal completely from their face, allowing them to inspire room air and necessitating PreOx to be recommenced, may better tolerate PreOx with a NRM supplemented by high flow nasal oxygen.
Beyond these specific contexts, however, the benefits of technique independence of mask application are lost. Firstly given that non-rebreather masks, when used in combination with high flow nasal O2 are able to provide a sufficiently high FiO2 for PreOx despite the absence of a seal around the mask (something they are unable to do in the absence of such a supplementary oxygen source), it stands to reason that small leaks around the face mask are also likely to be less significant with Mapleson/BVM masks when these are used in combination with high flow nasal oxygen. Thus when techniques for optimal ApOx are being implemented, these offset the impact of small leaks around either a NRM or a conventional face mask used with a BVM/Mapleson such that all of these become less technique independent. Secondly, technique independence comes at the cost of losing all the benefits outlined above with respect to “Automatic Checking”. Thirdly in sufficiently cooperative patients it is reasonable to expect that clinicians identifying themselves as airway experts are proficient at a basic skill such as achieving a seal with a face mask. This technique is critical to achieving ventilation with this device in apnoeic patients when other NSA techniques have failed. As such “airway experts” should not need to resort to a “technique independent” device in order to achieve effective PreOx.
11. Independence from Oxygen Supply:
Devices with a self-inflating bag retain the ability to ventilate the patient with room air if the oxygen supply fails. Whilst clearly a benefit in a pre-hospital environment or during intrahospital transport, this confers little advantage in other circumstances within a hospital where there is almost always an immediate backup supply of cylinder oxygen.
It is also important to recognise that again, this benefit comes at a price, as the ability of the bag to self-inflate without an ongoing oxygen supply removes a powerful cue for identifying oxygen failure (present with the collapse of a soft bag), when the oxygen supply is interrupted either by failure of wall/cylinder supply or (much more commonly) due to mis/disconnection of tubing from the oxygen source.
A summary of the performance of the 3 main devices in use for PreOx/ReOx outside of the operating suite, with respect to the above characteristics, is provided in the following table.
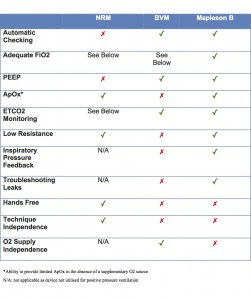 Click on image to enlarge.
Click on image to enlarge.
Discussion of Performance of Common O2 Delivery Devices with Respect to the Above Criteria:
Non-Rebreather Bag Mask with Supplemental Oxygen:

The NRM has limitations as an oxygen delivery device in the period surrounding advanced airway management according to the above criteria, largely as a consequence of it only being useful for PreOx but not ReOx.
Firstly it only supplies an adequate FiO2 for preoxygenation when combined with supplementary high-flow oxygen via the nasal or buccal routes (a desirable intervention which should be implemented for the purposes of ApOx anyway). Even with supplementary O2 an adequate FiO2 may not be sustained in the presence of significant patient hyperventilation.
Whilst the NRM allows for limited ApOx when it remains applied during the apnoeic period prior to laryngoscopy, this benefit becomes irrelevant when it is used in combination with supplementary nasal or buccal oxygen sources.
Although there are mechanisms that allow CO2 monitoring to be applied the NRM which satisfy the need to check that the CO2 sensor is present & operational, the other benefits of having CO2 connected to a face mask (assessment of seal and airway patency) cannot be yielded as this device is not used for subsequent positive pressure ventilation if this is required.
The resource sparing aspects of a “hands free” technique for PreOx are of questionable value and come at the cost of all the benefits listed under “Automatic Checking” above. As for technique independence, other than in the context of patient who is uncooperative/intolerant of a mask which requires a tight seal (which whilst potenially accounting for a signficant proportion of ED/ICU patients, is certainly not all of them) arguing for use of a NRM on the basis that it requires less technical skill is akin to arguing that emergency physicians should not learn direct laryngoscopy because it requires too much technical expertise and should instead default to videolaryngoscopy. Whilst NRM’s and videolaryngoscopes are useful techniques that will be adequate in many situations, in the truly difficult airway it is mastery of the basics that may separate the difficult intubation from a can’t intubate, can’t oxygenate (CICO) situation. Arguing for the use of a device that has other significant shortcomings on the basis that it does not require proficiency in technical skills considered fundamental to airway management is not a rationale worthy of clinicians considering themselves to be airway experts.
“In the truly difficult airway it is mastery of the basics that may separate the difficult intubation from a can’t intubate, can’t oxygenate (CICO) situation”
Conclusion: When combined with supplementary high flow buccal or nasal oxygen sources the NRM is an appropriate device for effective PreOx in situations where staff are very limited or where patients are intolerant of or uncooperative with having a tight face mask seal applied. Outside these contexts, however, it has a number of significant limitations which make devices which are also able to also be used for ReOx better suited to routine PreOx outside of the operating suite.
Self-Inflating Bag-Valve-Mask:

The self inflating bag-valve-mask device is probably the most common device used in the period surrounding advanced airway management. The defining feature and major advantage of the BVM is that the self inflating bag allows the generation of positive pressure for the purposes of ventilation even in the context of an interruption to the oxygen supply. This gives it clear advantages which outweigh its shortcomings in a pre-hospital environment and during intrahospital transport where rapid access to an alternative oxygen source may not be readily available. However, outside these contexts, where backup oxygen sources are readily available, the same self-inflating bag which makes it useful in pre-hospital & transport contexts results in significant disadvantages for the BVM.
“where backup oxygen sources are readily available, the same self-inflating bag which makes it useful in pre-hospital & transport contexts results in significant disadvantages for the BVM”
The adequacy of the FiO2 supplied is dependent on the device design and whether the patient is spontaneously ventilating or receiving positive pressure ventilation (as outlined in more detail here). These shortcomings are overcome, however, when supplementary nasal/buccal oxygen sources are implemented during PreOx for the purposes of subsequent ApOx. Even with supplementary O2, however, it may be possible for the FiO2 of BVM’s to fall below desirable levels for PreOx in the presence of significant hyperventilation.
The valves in the BVM prevent them acting as an oxygen source for the purposes of ApOx as they remain closed, preventing delivery of fresh gas, in the presence of apnoea (although again this disadvantage is overcome by application of supplementary oxygen which is necessary for optimal ApOx anyway) as well as providing significant resistance to inspiration in the spontaneously ventilating patient.
Finally the self inflating bag prevents distinction between primary & secondary face mask leaks whilst the stiffer material of which it is composed inhibits assessment of ventilation pressures.
It is worth noting that during spontaneous ventilation the reservoir bag of the BVM may give some clue as to the presence of face mask or equipment leaks, albeit with less sensitivity than the ventilation bag of a Mapleson. The reservoir bag of a BVM cannot, however, subsitute for the soft bag which is used for ventilation in the Mapleson B circuit as its emptying/refilling during PPV is dependent on different factors. The reservoir bag of the BVM empties due to compression of the self inflating component (thus giving an indication of the egress of gas from the device – whether this is into the airway or via a primary or secondary leak – and the correct functioning of the valves) and refills due to presence of an intact fresh gas supply. Thus the inflation/deflation of a BVM reservoir bag cannot be used to distinguish between primary & secondary face mask leaks.
Conclusion: In environments where a backup oxygen source may not be readily available, a self-inflating BVM is an appropriate choice for PreOx & ReOx, provided an appropriately designed device is chosen or the BVM is combined with a supplementary oxygen source (which also facilitates optimal ApOx). Outside these contexts, however, the BVM has some significant disadvantages in comparison with the Mapleson B, making it a less than ideal choice for PreOx/ReOx in most in-hospital situations.
Mapleson B:

The Mapleson B is a junctional reservoir system. It consists of a soft, collapsible reservoir bag at one end connected to a face mask at the opposite end by a segment of corrugated tubing. A pressure relief valve and the fresh gas inflow are located at the patient end of the circuit. Unlike self-inflating BVM devices, expired gas does not exit the device to the ambient air through a separate expiratory port but instead enters the device where it relies on the fresh gas flow (FGF) to wash it out of the pressure relief valve. Prevention of rebreathing depends on the balance between the FGF and the patient’s minute ventilation (MV) with rebreathing being prevented provided the FGF is > 2-2.5 times the MV. Once commonly used for advanced airway management outside of the operating theatre, particularly in the post-anaesthesia care unit, it has gradually undergone widespread replacement with the BVM – particularly since the introduction of disposable BVM devices.
The Mapleson performs well on the majority of the above criteria. In particular it continues to provide an adequate FiO2 for effective PreOx even in the presence of significant hyperventilation, where many NRM & BVM devices show a deterioration in FiO2 due to their ability to entrain room air in these circumstances.
The only criteria which the Mapleson doesn’t satisfy in the above table are those that are of questionable value. A hands free technique may be of benefit when staffing resources are very limited but carries with it the risk of distracting the airway operator from the vigilant monitioring of the patient’s airway & breathing status in the lead up to definitive airway management. As described above the significance of technique independence is presumably mitigated when supplementary O2 sources for the purposes of ApOx are implemented (and this is the only context in which comparison with a NRM can be made with the Mapleson B, as without supplementary O2 the NRM is unable to meet the fundamental criterion of adequacy of FiO2 for effective PreOx). Independence from O2 supply is irrelevant for most in-hospital use (other than intrahospital transport) due to the ready availability of backup oxygen supplies.
The most frequent criticisms of the Mapleson B are that it requires greater technical expertise and that it allows rebreathing:
- Technical expertise: the only added complexity of the Mapleson B is the presence of an adjustable pressure limiting valve – essentially a PEEP valve which covers a much wider range of pressures (from zero to around 70cmH2O). This is a useful feature which requires very little practice for the user to become comfortable with it. Since the same face masks used with a BVM can be used with a Mapleson, the only other technical expertise is that required to achieve an effective face mask seal. For the reasons discussed above it is unreasonable for clinicians without the skills to achieve a face mask seal to be independently engaging in advanced airway management in the first instance. The erroneous notion that achieving a seal is more difficult with a Mapleson derives from the fact that, as described above, whilst the self-inflating bag of a BVM conceals poor face mask technique, the collapse of the soft bag of a Mapleson provides a sensitive mechanism to reveal when an inadequate seal has been achieved. With both devices face mask ventilation will not be possible when the seal is inadequate – the BVM simply disguises the fact that an inadequate face mask seal is present (primary leak) and allows the airway operator to believe that the problem lies with an obstructed airway (secondary leak).
- Rebreathing: the issue of rebreathing is purely academic. Rebreathing of itself is not of any clinical significance unless it leads to hypercapnia. Since rebreathing with a Mapleson B only occurs if the MV is more than 50% of the FGF (which would be at least 20L/min with standard oxygen rotameters “overcranked” beyond the marked calibrations) this would require the patient to have a MV >10L/min which would result in them being hypocapnic in the absence of significant hypermetabolism. Even then, hypercapnia & acidosis is well tolerated in many patients. Elective surgical patients spontaneously breathing on an laryngeal mask not infrequently achieve ETCO2 values in excess of 60mmHg without ill effects. Whilst pre-existing acidosis, electrolyte disturbances, myocardial depression or raised intracranial pressure, conditions not infrequently present in critically unwell patients, may limit a patient’s tolerance to hypercapnia it is apparent that the occurence of rebreathing with a Mapleson is only significant if the patient’s MV is >10L/min in the presence of significant hypermetabolism and comoribidities which make hypercarbia undesirable. This represents a minority of patients and these can easily be avoided by routine use of ETCO2 monitoring during PreOx and substituting a different device for the Mapleson B if the ETCO2 is above desirable levels.
“it is unreasonable for clinicians without the skills to achieve a face mask seal to be independently engaging in advanced airway management… the BVM simply disguises the fact that an inadequate face mask seal is present”
Conclusion: The Mapleson B has many advantages over the NRM & BVM and no significant disadvantages in most circumstances. For most in-hospital use in patients outside of the operating theatre, who will tolerate a firmly applied mask, it is unquestionably the most appropriate PreOx/ReOx device for use during the period surrounding advanced airway management, provided adequate staff are available to apply it and backup oxygen sources are immediately available.